The What & Why
This section provides foundational knowledge about migraines. Understanding what's happening in your body is the first step toward effective management. Explore the tabs below to learn about the nature of migraines, different types, and their phases.
Understanding Migraines
Migraine Types
Migraine with Aura: Preceded by visual disturbances like flashing lights, zig-zag lines, or blind spots.
Migraine without Aura: The most common type, without the preceding sensory disturbances.
Episodic Migraine: Less than 15 headache days a month, can have infrequent attacks (once or twice a year) or more frequent attacks (several times a week)
Chronic Migraine: Headaches on 15 or more days a month, with at least 8 having migraine features.
Vestibular Migraine: Characterized by vertigo and dizziness, sometimes without a significant headache.
Retinal Migraine: Brief loss of vision in one eye. Can seeing flashing lights or wavy lines. Headache may or may not be present
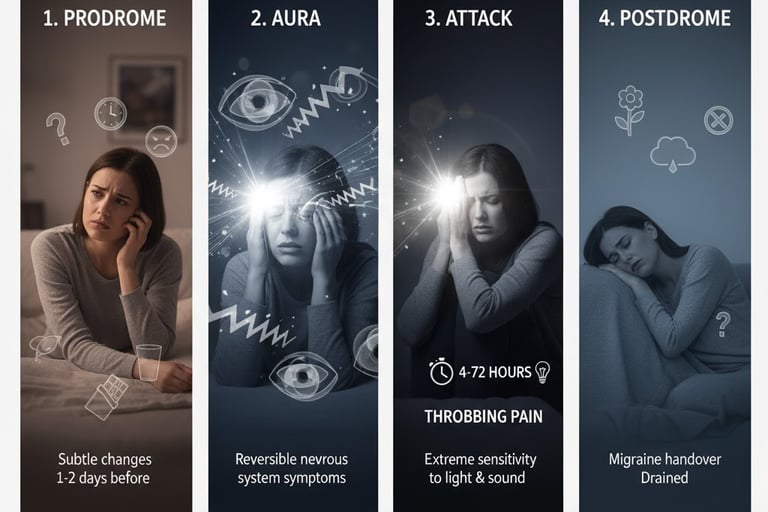
Migraine Phases
Prodrome: Subtle changes 1-2 days before a migraine, like mood changes or food cravings.
Aura: Reversible symptoms of the nervous system, usually visual, that precede the headache.
Attack: The headache phase, with throbbing pain and other symptoms, lasting 4 to 72 hours.
Postdrome: The "migraine hangover" phase after an attack, where you may feel drained or confused.
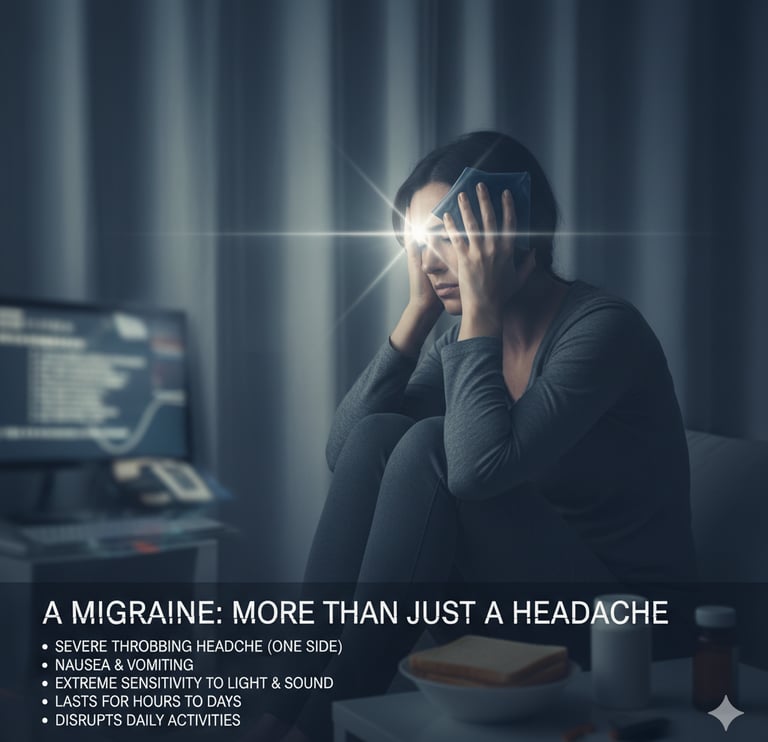
A Neurological Condition, Not "Just a Headache"
A migraine is a complex neurological disease that causes moderate to severe pain, typically on one side of the head. Unlike a tension headache, it's often accompanied by other symptoms like nausea, vomiting, and extreme sensitivity to light and sound. The pain often feels throbbing or pulsing and can last for hours to days. The pain can be so severe that it interferes with your daily activities.
Doctors believe migraines happen because of changes in the brain and nerves, especially the trigeminal nerve, which affects blood vessels in the head.
What is a Migraine?

Other Headache Types:
1. Tension Headache
This is the most common type of headache.
What it feels like: A dull, aching pain or pressure on both sides of your head. Many people describe it as feeling like a tight band is wrapped around their head. The pain is usually mild to moderate. You may also feel tenderness in your scalp, neck, and shoulder muscles.
Common Causes & Triggers: Stress is the most common trigger. Others include poor posture, eye strain (like from long hours at a computer), fatigue, and lack of sleep.
2. Sinus Headache
This type is caused by swelling and inflammation in your sinuses (the air-filled cavities in your face).
What it feels like: A deep, constant, aching pain in your cheekbones, forehead, and the bridge of your nose. The pain often gets worse when you bend forward or lie down.
Other Symptoms: You will almost always have other sinus symptoms, such as a runny or stuffy nose, thick, discolored nasal discharge, fever, and a feeling of fullness in your ears.
Common Causes & Triggers: A sinus infection (sinusitis) or allergies.
3. Medication Overuse Headache (Rebound Headache)
This headache is caused by frequently taking pain medication to treat headaches.
What it feels like: A persistent, daily, or near-daily headache. It is often present as soon as you wake up in the morning.
Common Causes & Triggers: Regularly taking over-the-counter pain relievers (like acetaminophen, ibuprofen, or aspirin) more than 15 days a month, or taking prescription headache medicines (like triptans) more than 10 days a month. Your body gets used to the medication, and you get a "withdrawal" headache when the medicine wears off.
4. Cervicogenic Headache
This is a "secondary" headache, meaning the pain is referred from a problem in your neck.
What it feels like: Pain that starts at the base of your skull or in your neck and radiates up to one side of your head, often to the front. The pain is usually a non-throbbing, steady ache.
Other Symptoms: You may have a stiff neck and find that your headache gets worse with certain neck movements.
Common Causes & Triggers: An underlying issue in the cervical (neck) spine, such as arthritis, a "pinched" nerve, or an old injury like whiplash.
5. Exertion Headache
This is a headache brought on by sudden, intense physical activity.
What it feels like: A short-lived, throbbing headache that occurs on both sides of your head during or immediately after strenuous exercise.
Common Causes & Triggers: Any form of intense activity, such as running, weightlifting, or sexual intercourse.
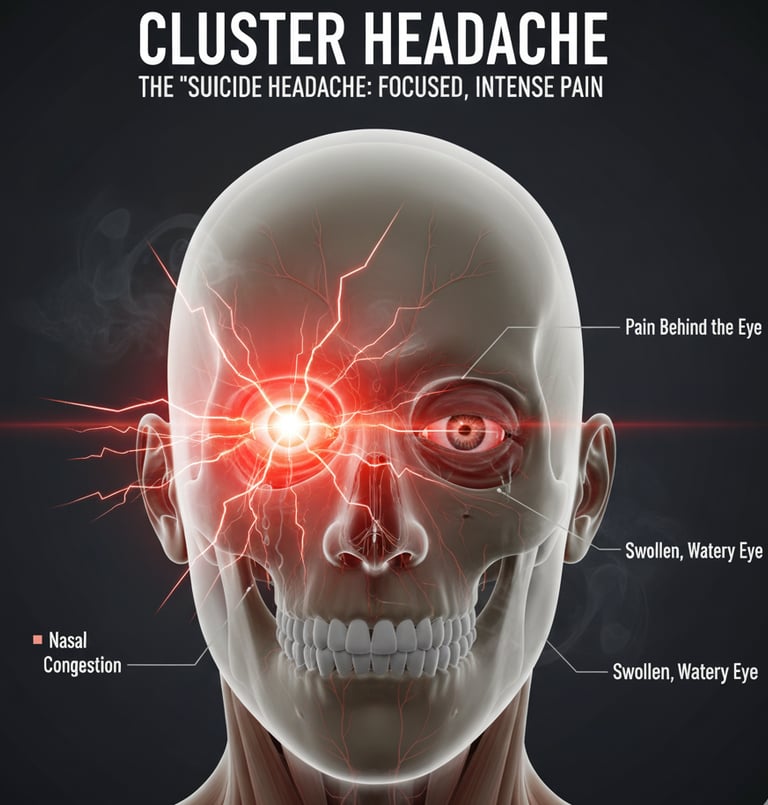
6. Cluster Headache
These are rare but extremely painful headaches that occur in "clusters,"
meaning you get them in groups over a period of weeks or months.
What it feels like: A severe, sharp, burning, or piercing pain on
one side of the head. It is almost always located in or around one eye.
The pain is so intense that most people cannot sit still during an attack.
Other Symptoms: On the same side as the pain, you will likely have a red,
watery eye, a drooping or swollen eyelid, and a runny or stuffed nostril.
Common Causes & Triggers: The exact cause is unknown.
Alcohol and smoking can often trigger an attack during a cluster period.
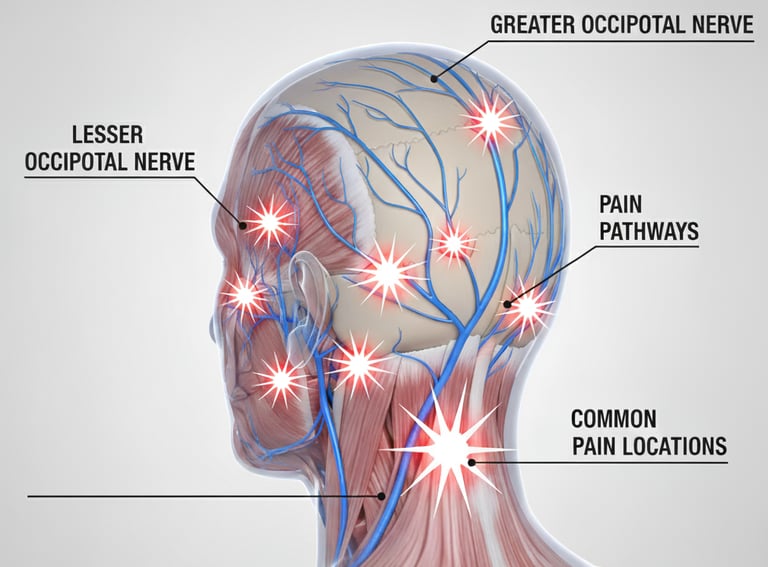
7. Occipital Neuralgia
This is a headache caused by irritation or injury to the occipital nerves, which run from the top of your spinal cord up to your scalp.
What it feels like: A sharp, jabbing, electric shock-like pain. It typically starts at the base of your skull and radiates up one side of your head or to the back of your head. The attacks of pain are often brief, lasting seconds to minutes.
Other Symptoms: The scalp can become extremely tender to the touch, and even brushing your hair or laying on a pillow can trigger the pain. Some people also feel pain behind their eye on the affected side.
Common Causes & Triggers: Often caused by a pinched nerve in the neck, osteoarthritis, tight neck muscles, or head/neck trauma (like whiplash).